What Is PCOS? A Hormone-Based Explanation (Beyond the Ovaries)
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal conditions affecting women, yet it is also one of the most misunderstood.
Many women are told PCOS is an “ovarian problem” or are shown an ultrasound with cysts and sent home with a prescription for birth control. While this explanation is common, it is incomplete.
PCOS is not just a gynecologic condition.
It is a neuro-endocrine-metabolic condition that affects the entire body.
Understanding this changes everything, from treatment options to long-term outcomes.
Why the “Ovary-Only” Explanation Falls Short
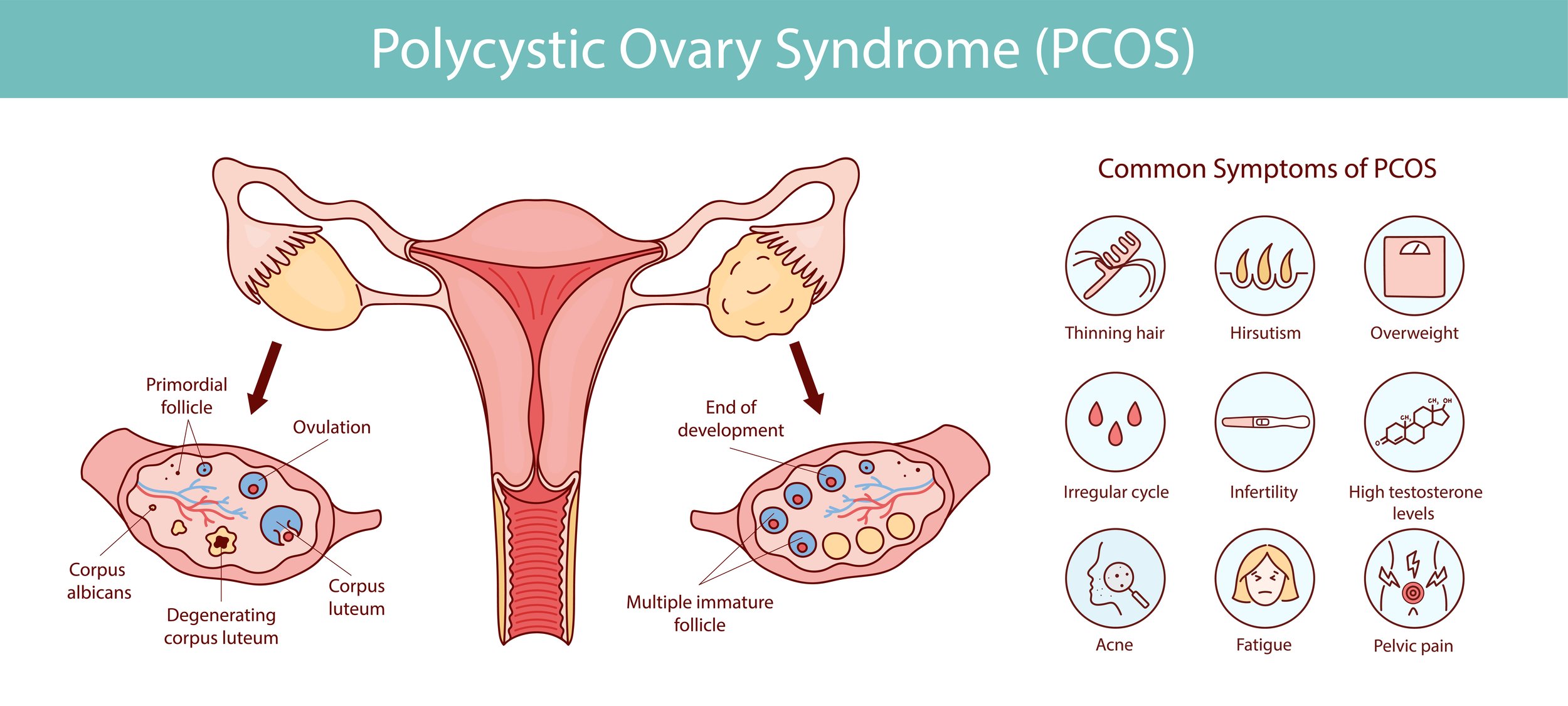
The traditional diagnostic criteria for PCOS include:
Irregular or absent ovulation
Signs of elevated androgens (such as testosterone)
Polycystic-appearing ovaries on ultrasound
However:
You can have PCOS without cysts
You can have cysts without PCOS
Treating the ovaries alone does not resolve the condition
This is because the ovaries are responding to signals coming from elsewhere.
PCOS as a Neuro-Endocrine-Metabolic Condition
To understand PCOS properly, we need to look at three interconnected systems.
1. The Neuro (Brain) Component
The hypothalamus and pituitary gland regulate hormone signaling through pulses of LH and FSH.
In PCOS, this signaling is often disrupted, leading to:
Poor follicle development
Lack of ovulation
Imbalanced hormone output
Stress, under-eating, over-exercise, and chronic cortisol elevation all interfere with this signaling.
2. The Endocrine (Hormone) Component
PCOS affects multiple hormones simultaneously:
Insulin (often elevated or poorly regulated)
Androgens (testosterone, DHEA)
Estrogen (often present but poorly cleared)
Progesterone (low due to lack of ovulation)
Cortisol (chronically elevated in many women)
This is why PCOS symptoms extend far beyond the reproductive system.
3. The Metabolic Component
PCOS is strongly associated with:
Insulin resistance
Blood sugar instability
Increased inflammation
Even women who are lean can have metabolic dysfunction.
This is why PCOS is now recognized as a metabolic condition with reproductive manifestations, not the other way around.
Why Symptoms Look So Different From Woman to Woman
Some women struggle with:
Acne and hair growth
Weight gain
Anxiety and fatigue
Others experience:
Irregular cycles only
Infertility without obvious metabolic symptoms
These differences exist because PCOS is not one condition with one cause.
Which brings us to the most important concept in PCOS care.
The Takeaway
PCOS is not “just a period problem”
PCOS is not “just an ovary problem”
PCOS is a whole-body condition driven by hormone communication, metabolism, and stress physiology
When we treat it that way, outcomes improve.
Ready for a Deeper PCOS Assessment?
If you’ve been told your labs are normal or your only option is birth control, a hormone-focused approach may offer clarity.
PCOS is not one-size-fits-all, and neither is care.